Change settings Select a country and language to get personalized content
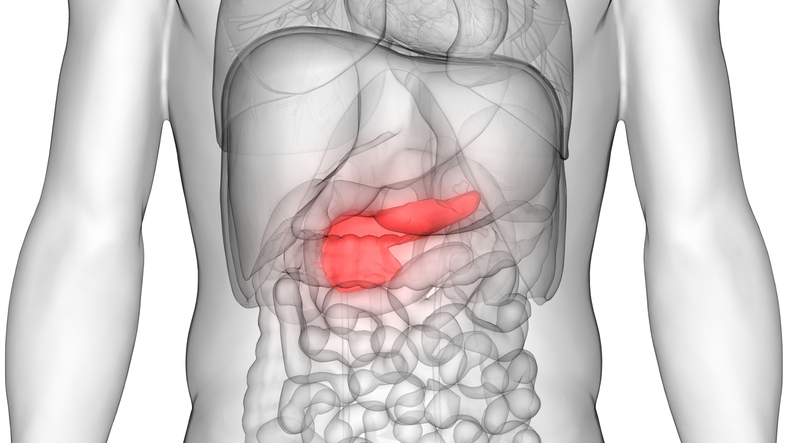
Pancreatitis - Symptoms, Treatment, and Prevention
Pancreatitis is an inflammation of the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen.
The pancreas produces enzymes that aid digestion and hormones that help regulate how your body processes sugar (glucose).
Pancreatitis can occur as acute pancreatitis, which means it comes on suddenly and lasts for days. Some people develop chronic pancreatitis, which is pancreatitis that occurs over many years.
Mild cases of pancreatitis improve with treatment, but severe cases can cause life-threatening complications.
Symptoms

The signs and symptoms of pancreatitis can vary depending on the type you have.
Signs and symptoms of acute pancreatitis include:
- Pain in the upper abdomen
- Pain in the abdomen that radiates to the back
- Tenderness when touching the abdomen
- High temperature
- Rapid pulse
- Nausea
- Vomiting
Signs and symptoms of chronic pancreatitis include:
- Pain in the upper abdomen
- Abdominal pain that worsens after eating
- Weight loss without cause
Causes

Pancreatitis occurs when digestive enzymes are activated while still in the pancreas, irritating the cells of the pancreas and causing inflammation.
Repeated attacks of acute pancreatitis can damage the pancreas and lead to chronic pancreatitis. Scar tissue can form in the pancreas, leading to loss of function. A poorly functioning pancreas can cause digestive problems and diabetes.
Conditions that can lead to acute pancreatitis include:
- Gallstones
- Alcoholism
- Certain medications
- High levels of triglycerides in the blood (hypertriglyceridemia)
- High levels of calcium in the blood (hypercalcemia), which can be caused by an overactive parathyroid gland (hyperparathyroidism)
- Pancreatic cancer
- Abdominal surgery
- Cystic fibrosis
- Infection
- Abdominal injury
- Obesity
- Trauma
Endoscopic retrograde cholangiopancreatography, a procedure used to treat gallstones, can also lead to pancreatitis.
Sometimes the cause of pancreatitis is never found. This is known as idiopathic pancreatitis.
Risk factors
Factors that increase the risk of pancreatitis include:
- Excessive alcohol consumption. Studies show that heavy drinkers (people who consume four to five drinks a day) are at increased risk for pancreatitis.
- Cigarette smoking. Smokers are on average three times more likely to develop chronic pancreatitis than non-smokers. The good news is that quitting smoking reduces the risk by about half.
- Obesity. You are more likely to develop pancreatitis if you are overweight.
- Diabetes. Diabetes increases the risk of pancreatitis.
- Family history of pancreatitis. The role of genetics is becoming increasingly recognized in chronic pancreatitis. If you have family members with this condition, your chances increase—especially when combined with other risk factors.
Complications
Pancreatitis can cause serious complications, including:
- Kidney failure. Acute pancreatitis can cause kidney failure, which can be treated with dialysis if the kidney failure is severe and prolonged.
- Breathing problems. Acute pancreatitis can cause chemical changes in your body that affect your lung function, causing the oxygen level in your blood to drop to dangerously low levels.
- Infection. Acute pancreatitis can make your pancreas vulnerable to bacteria and infection. Infections of the pancreas are serious and require intensive treatment, such as surgery to remove the infected tissue.
- Pseudocyst. Acute pancreatitis can lead to fluid and debris collecting in cyst-like pockets in the pancreas. A large pseudocyst that ruptures can cause complications such as internal bleeding and infection.
- Malnutrition. Both acute and chronic pancreatitis can cause your pancreas to produce fewer of the enzymes needed to break down and process nutrients from the food you eat. This can lead to malnutrition, diarrhea, and weight loss, even though you may be eating the same foods or the same amount of food.
- Diabetes. Damage to the insulin-producing cells in your pancreas from chronic pancreatitis can lead to diabetes, a disease that affects how your body uses blood sugar.
- Pancreatic cancer. Long-term inflammation of the pancreas caused by chronic pancreatitis is a risk factor for developing pancreatic cancer.
Diagnosis
Tests and procedures used to diagnose pancreatitis include:
- Blood tests to look for elevated levels of pancreatic enzymes, along with white blood cells, kidney function, and liver enzymes
- Abdominal ultrasound to look for gallstones and inflammation of the pancreas
- Computed tomography to look for gallstones and assess the degree of inflammation of the pancreas
- Magnetic resonance imaging to check for abnormalities in the gallbladder, pancreas, and ducts
- Endoscopic ultrasound to check for inflammation and blockages in the pancreatic duct or bile duct
- Stool tests in chronic pancreatitis to measure fat levels, which could indicate that your digestive system is not absorbing nutrients properly
Treatment
Initial treatment in the hospital may include:
- Early feeding. Older data suggested that you should stop eating for a few days in the hospital to give your pancreas a chance to recover. This is no longer practiced. More recent data suggests that eating as soon as you can tolerate food helps the pancreas heal.
As the inflammation in your pancreas improves, you should start drinking clear liquids and eating soft foods. Over time, you can return to your normal diet.
If your pancreatitis symptoms continue and you still experience pain when eating, your doctor may recommend a feeding tube to help you get nutrition. - Pain relievers. Pancreatitis can cause severe pain. Your healthcare team will give you medication to help you manage the pain.
- Intravenous fluids. Because your body is expending energy and fluids to repair your pancreas, you may become dehydrated. For this reason, you will receive extra fluids through a vein in your arm during your hospital stay.
Once your pancreatitis is under control, your healthcare team will evaluate and treat the underlying cause of your pancreatitis. Depending on the cause of your pancreatitis, treatment may include:
- Procedures to remove blockages in the bile ducts. Pancreatitis caused by a narrowed or blocked bile duct may require procedures to open or widen the bile duct.
A procedure called endoscopic retrograde cholangiopancreatography uses a long tube with a camera at the end to examine the pancreas and bile ducts. The tube is passed through your throat, and the camera sends images of your digestive system to a monitor. Anesthesia is used for this procedure.
Endoscopic retrograde cholangiopancreatography can help diagnose problems in the bile duct and pancreatic duct and remove obstructions, such as gallstones. However, in some people, it can also lead to acute pancreatitis. - Gallbladder surgery. If gallstones have caused pancreatitis, your doctor will recommend surgery to remove the gallbladder (cholecystectomy).
- Pancreatic procedures. Endoscopic procedures may be necessary to drain fluid from the pancreas or remove diseased tissue.
- Alcohol dependence treatment. Drinking several alcoholic beverages a day for many years can cause pancreatitis. If this is the cause of your pancreatitis, your doctor may recommend that you enter an alcohol dependence treatment program. Continuing to drink alcohol would worsen your pancreatitis and lead to serious complications.
- Medication changes: If a medication is thought to be causing acute pancreatitis, your doctor may stop the medication and work with you to find alternatives.
Additional Treatments for Chronic Pancreatitis
Depending on your situation, chronic pancreatitis may require additional treatments, including:
- Pain management. Chronic pancreatitis can cause persistent abdominal pain. Your doctor will assess the causes of your chronic pancreatitis and may recommend medications to control your pain.
Severe pain may be relieved with options such as endoscopic ultrasound or injections to block the nerves that send pain signals from the pancreas to the brain. - Enzymes to improve digestion. In chronic pancreatitis leading to diarrhea or weight loss, pancreatic enzyme supplements can help your body break down and process the nutrients in the foods you eat. Pancreatic enzymes are taken with each meal.
- Changes to your diet. Your doctor may refer you to a dietitian who can help you plan meals with low-fat foods that are high in nutrients.
After you leave the hospital, you can take steps to continue your recovery from pancreatitis, such as:
- Stop drinking alcohol. Even if alcohol is not considered a cause of acute pancreatitis, it is wise to stop drinking alcohol while you are recovering. If you cannot stop drinking alcohol on your own, ask your doctor for help. Your doctor can refer you to programs that can help you stop drinking.
- Stop smoking. If you smoke, quit. If you don't smoke, don't start. If you can't quit on your own, ask your doctor for help. Medications and counseling can help you quit smoking.
- Choose low-fat foods. Choose foods that limit fat and emphasize fresh fruits and vegetables, whole grains, and lean proteins.
- Drink more fluids. Pancreatitis can cause dehydration, so drink more fluids throughout the day. It may help to carry a water bottle or cup of water with you.
Alternative Medicine

Alternative therapies cannot cure pancreatitis, but some alternative therapies may help you manage the pain associated with pancreatitis.
People with chronic pancreatitis may experience ongoing pain that is not easily controlled with medication. Using complementary and alternative medical therapies along with the medications prescribed by your doctor may help you feel more in control of your pain.
Examples of alternative therapies that may help you manage your pain include:
- Meditation
- Relaxation exercises
- Yoga
- Acupuncture
Preparing for Your Appointment
Start by visiting your family doctor or general practitioner if you have signs or symptoms that concern you. If your doctor suspects you may have pancreatitis, you may be referred to a doctor who specializes in the digestive system (gastroenterologist).
Since appointments can be brief and there is often a lot to discuss, it is a good idea to be well prepared. Here is some information to help you prepare and know what to expect from your doctor.
What Can You Do?
- Be aware of any restrictions before making an appointment. When you make your appointment, be sure to ask if there is anything you need to do in advance, such as restricting your diet.
- Write down all the symptoms you are experiencing, including those that may seem unrelated to the reason you scheduled the appointment.
- Write down key personal information, including any major stressors or recent life changes.
- Make a list of all medications, as well as any vitamins or supplements you are taking.
- Bring a family member or friend with you. It can sometimes be difficult to absorb all the information provided during an appointment. Someone accompanying you may remember something you missed or forgot.
- Write down questions to ask your doctor.
For pancreatitis, some basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- What are other possible causes of my symptoms or condition?
- What types of tests do I need?
- Is my condition temporary or chronic?
- What is the best course of action?
- I have other health problems. How can I best manage pancreatitis along with these conditions?
- Are there any restrictions I need to follow?
- Do I need to see a specialist? How much will this cost, and will my insurance cover it?
- What will determine whether I need to schedule a follow-up visit?
In addition to the questions you have prepared to ask your doctor, don't hesitate to ask other questions.
What to Expect from Your Doctor
Your doctor will probably ask you a number of questions. If you are prepared to answer them, this may allow you more time to cover the points you want to discuss. Your doctor may ask:
- When did you first start experiencing symptoms?
- Are your symptoms ongoing or intermittent?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to make your symptoms worse?
- Have you had these symptoms before?
- Have you been diagnosed with pancreatitis in the past?
- Do you drink alcohol? If so, how much and how often do you drink?
- Did you start any new medications before your symptoms began?
- Is there a family history of pancreatic disease?
















